In the medical field, acronyms are very popular. If you have chronic obstructive pulmonary disease (COPD), you may visit your doctor to determine whether you require long-term oxygen therapy or continuous positive airway pressure (CPAP) (LTOT). We can gain valuable time throughout our demanding workload by using acronyms. Unfortunately, when medical terminology interferes with a patient’s comprehension of their condition, it can cause a lot of confusion.
COLDOSA, the mother of all medical abbreviations (Chronic Obstructive Lung Disease and Obstructive Sleep Apnoea). Fortunately, we can simplify this for our perplexed patients by naming it Overlap Syndrome, or OS.
When a patient has both chronic obstructive pulmonary disease and obstructive sleep apnea, it is referred to as overlap syndrome, or COLDOSA. When these disorders are present together, the amount of oxygen in the blood during sleep significantly decreases, increasing the risk of impairment and death.

How can COPD overlap with OSA?
The term “overlap” may imply that COPD sufferers share certain traits, but in this instance, the term is misleading. Instead, these are two widely prevalent, distinct disorders that each have a distinctive effect on your airways. The “overlap” in a person with both conditions refers to how the conditions combine to raise the risks above and above what would be anticipated for each ailment.
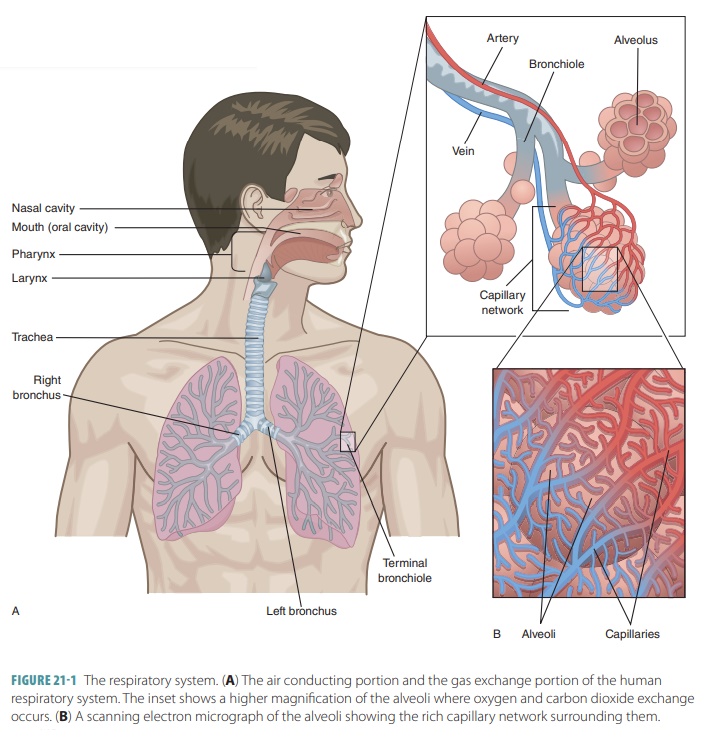
With COPD, which is typically brought on by smoking, your lungs’ alveoli gradually get blocked off from airflow as a result of persistent inflammation. Simply put, breathing in smoke or other toxic fumes causes irritation in the lungs, which results in an irreversible constriction of the airways and makes breathing more difficult. The mortality and morbidity rates for COPD are high.
Another prevalent condition is obstructed sleep apnoea (OSA), which occurs when the throat’s muscles relax while you sleep and cause your airway to occasionally close. This is accompanied by loud snoring and rapidly decreasing oxygen levels while you sleep, which eventually causes a startling wakeup. This increases the risk of high blood pressure, heart disease, and stroke while also causing disrupted sleep and increased daytime sleepiness.
Both COPD and OSA are extremely prevalent diseases; in the UK, 1.5 million people have been diagnosed with OSA and 1.17 million with COPD, respectively. The true prevalence of both COPD and OSA in individuals over 40 is considered to be between 5 and 10%; this figure only represents the number of patients who have received a diagnosis.
How can this syndrome affect your health?
The muscles in our upper airway, diaphragm, and chest wall relax as we sleep, especially during the rapid eye movement (REM) phase. Typically, this doesn’t pose a big issue, and we can still get a good night’s sleep.
This deep sleep is almost impossible for patients with OSA because during REM sleep, the relaxed upper airway fully closes. This is brought on by increased throat pressure from conditions including obesity and peripheral oedema, as well as constricted airways from nasal congestion or larger tonsils. You become unable to breathe when the airway closes, which results in hypoxia (low oxygen levels), until the brain’s sensors kick in and awaken you. As a result, there are frequent instances of low oxygen levels throughout the night, arousals, and disrupted sleep.
Patients with COPD also experience comparable issues with sleep quality. As a result of lung scarring and airway constriction, the lungs are unable to adjust for the chest wall’s decreased mobility during REM sleep, rendering breathing ineffective. 70% of COPD patients are reported to experience a reduction in oxygen levels during night, and nearly half of patients with COPD report having trouble falling or staying asleep.
When OSA and COPD interact, it causes even more interrupted sleep and frequently occurs nocturnal hypoxaemia, or low oxygen levels at night. For unfathomable reasons, these impacts work in concert, and the overall risks outweigh the individual ones.
Short-term symptoms of nocturnal hypoxaemia include weariness, lack of focus, and daytime somnolence (sleepiness). However, the long-term consequences of persistent nocturnal hypoxaemia are where the actual danger lies. An extended drop in oxygen levels stimulates the body’s inflammatory response, which is repeated several times each night and eventually results in a chronic state of inflammation. Inflammation in this stage can result in a number of conditions, including:
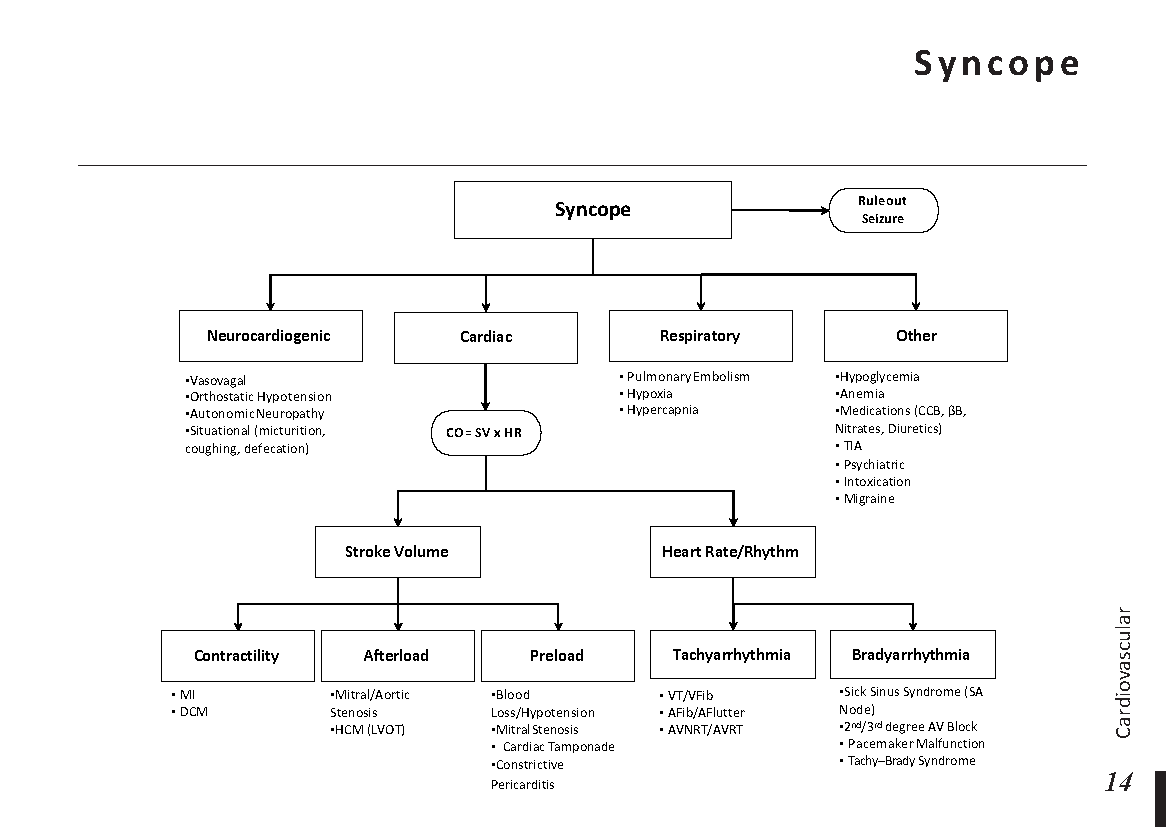
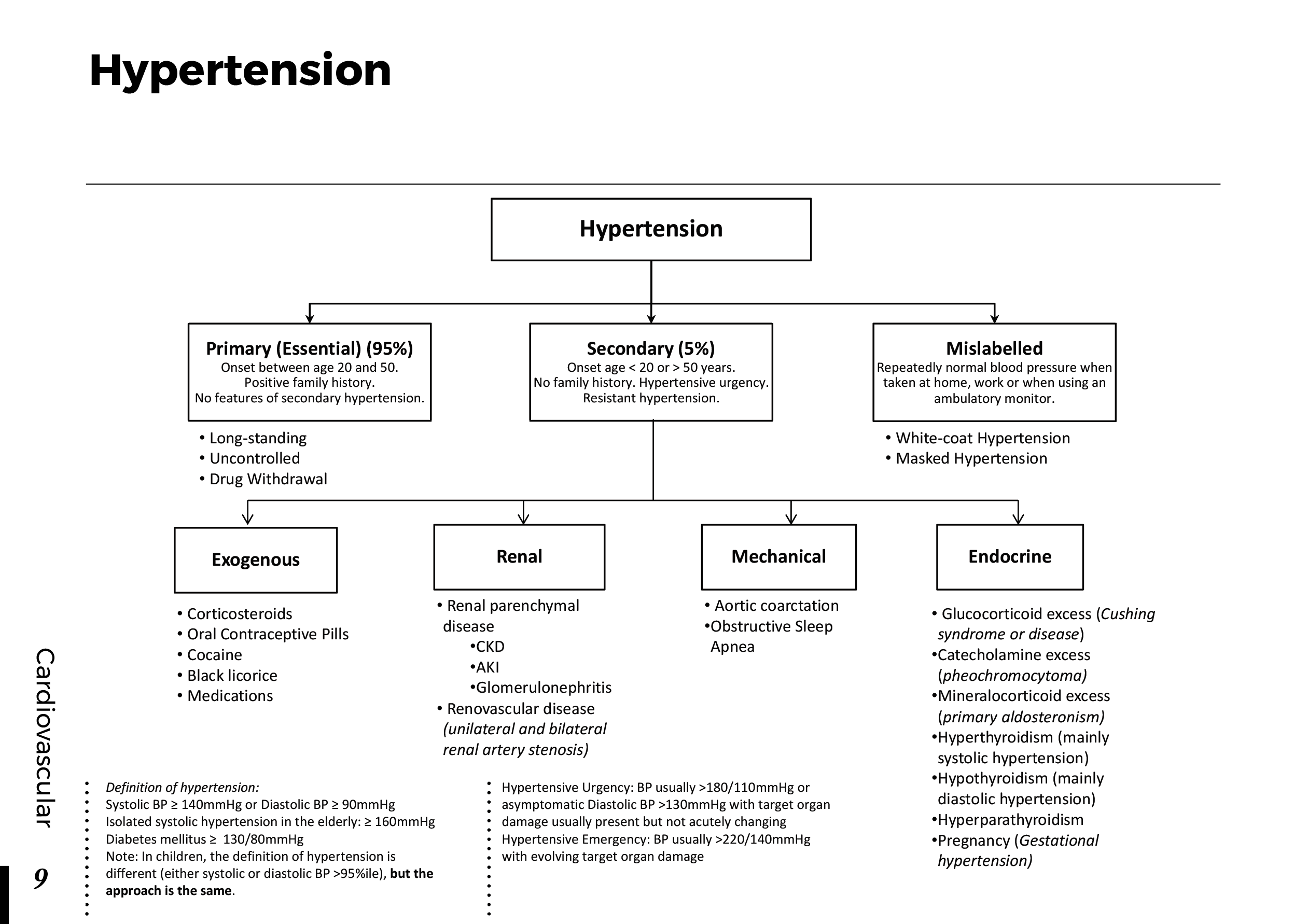
- Hypertension
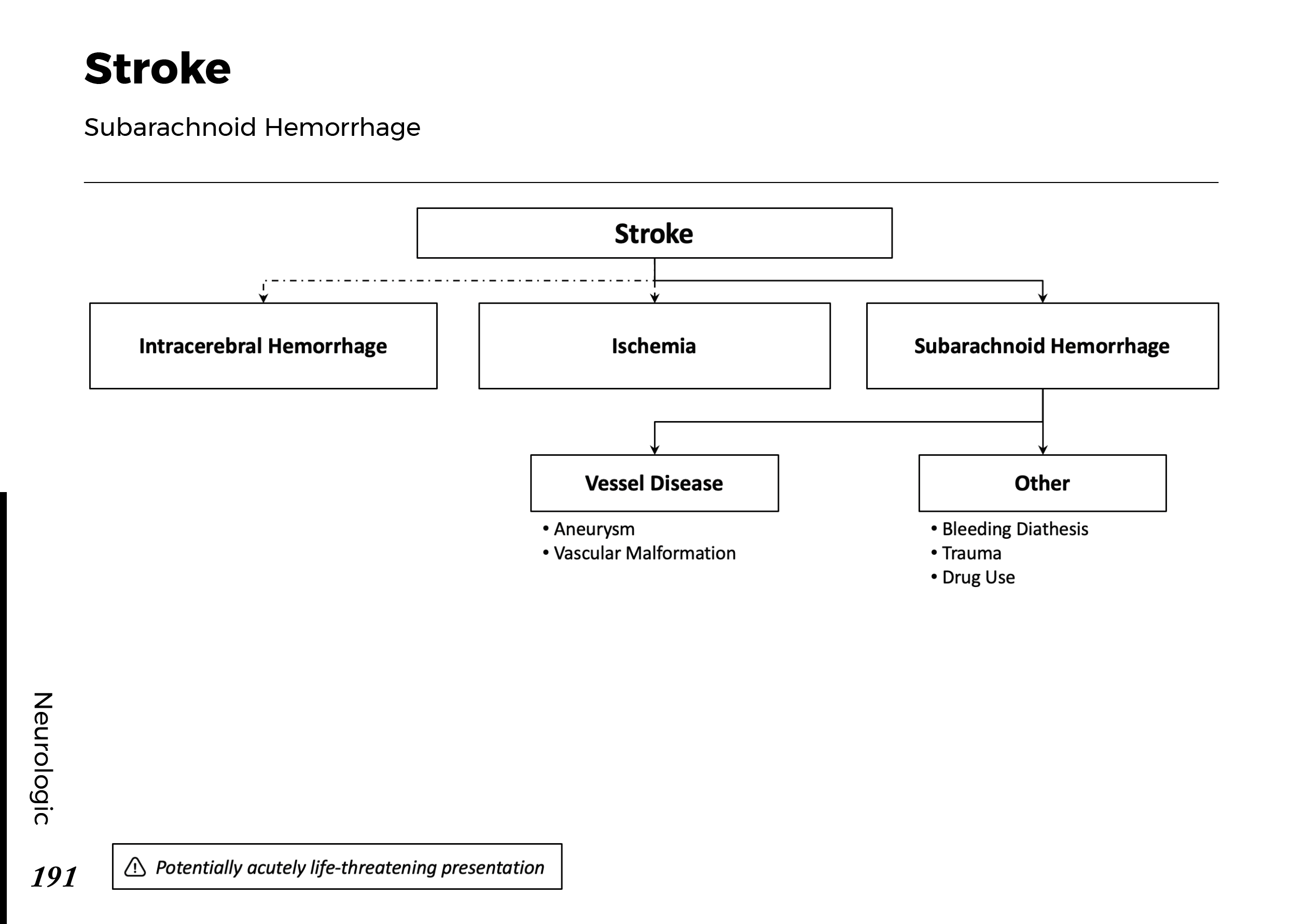
- Stroke
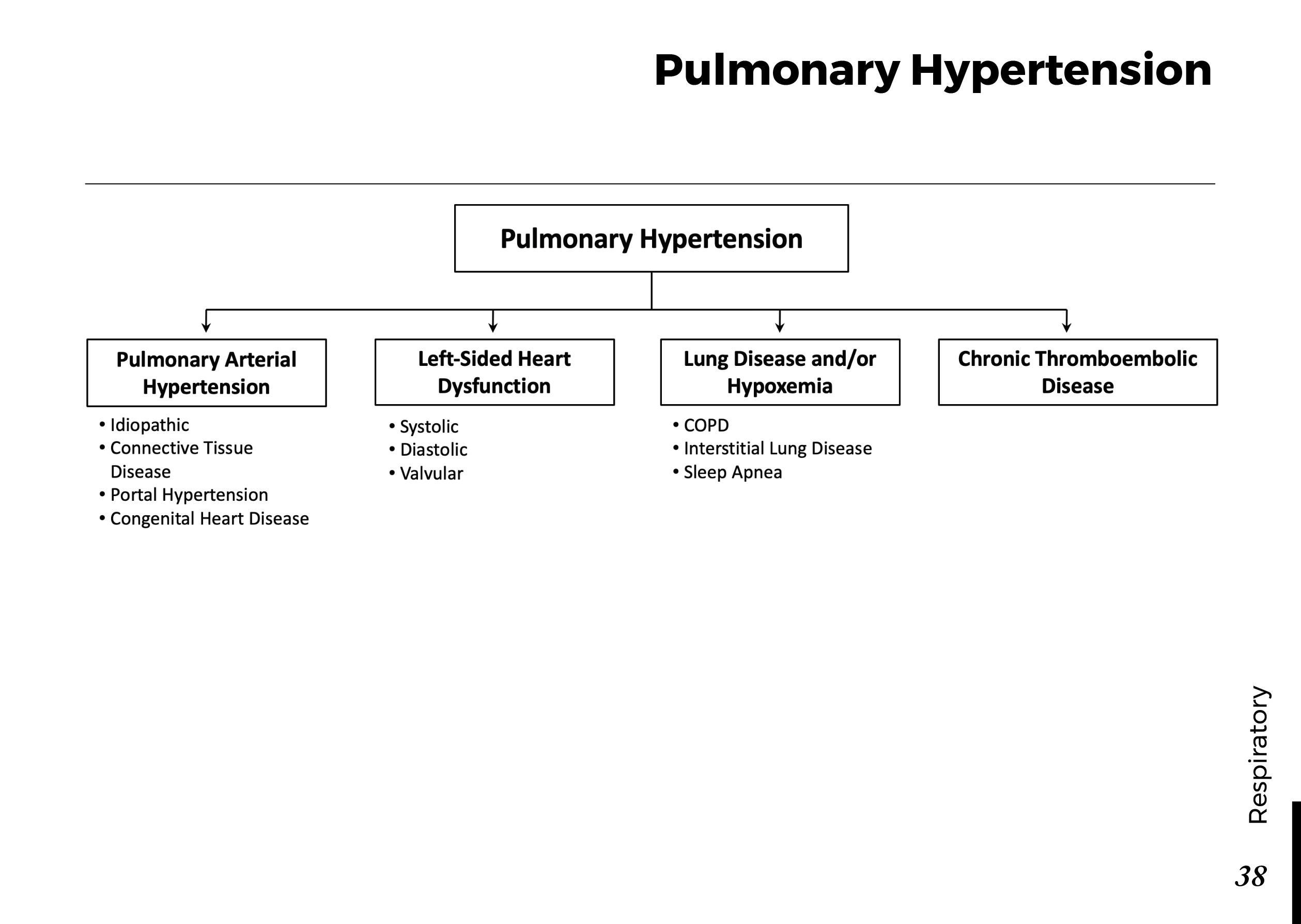
- Pulmonary Hypertension
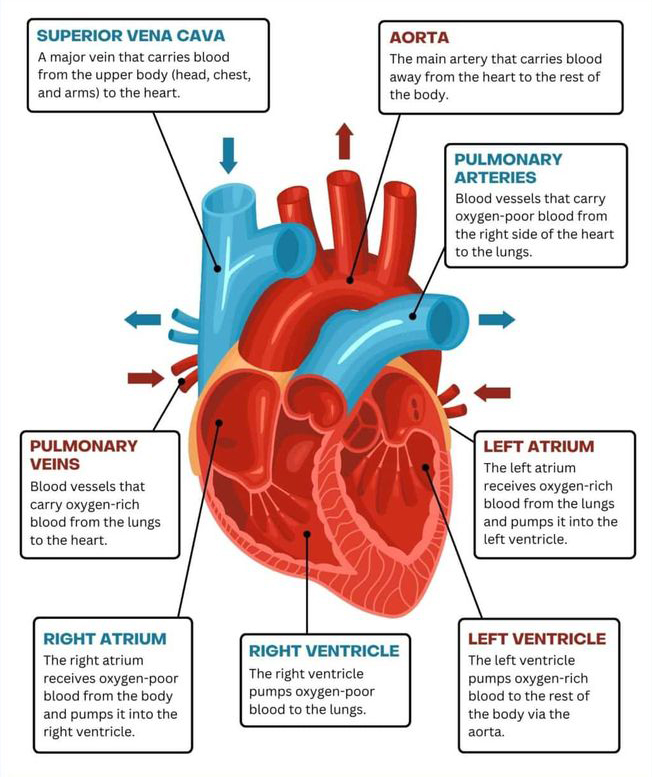
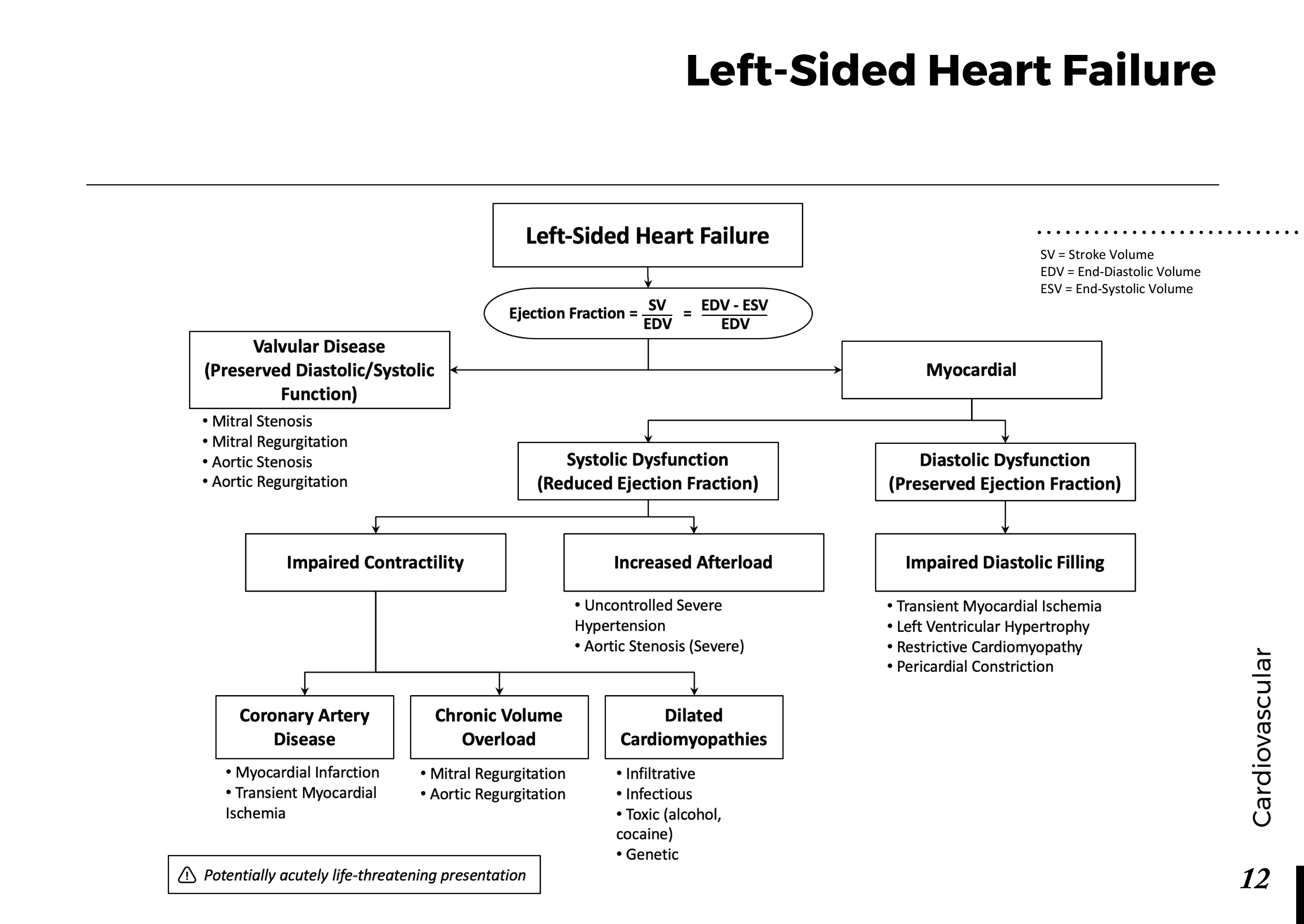
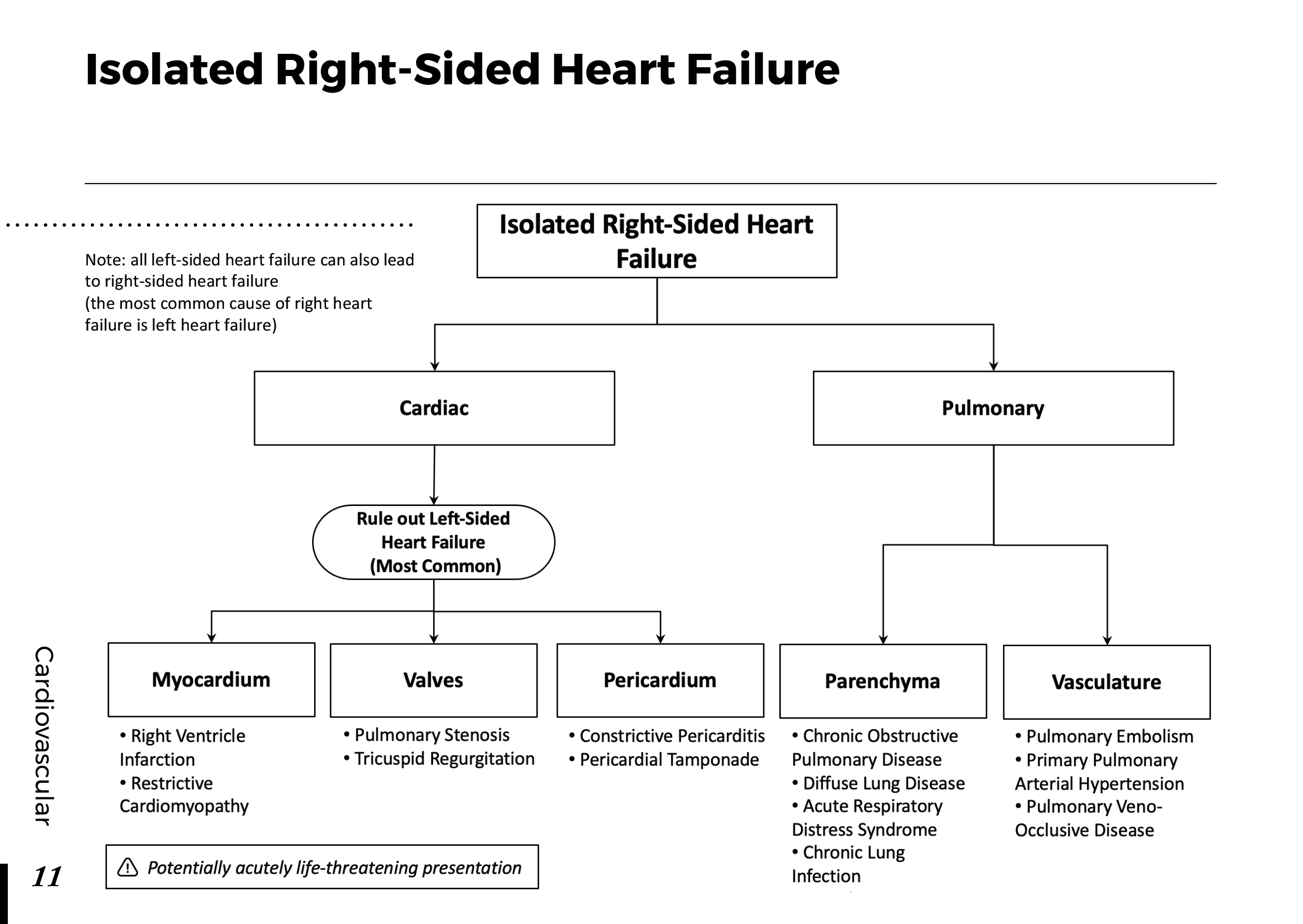
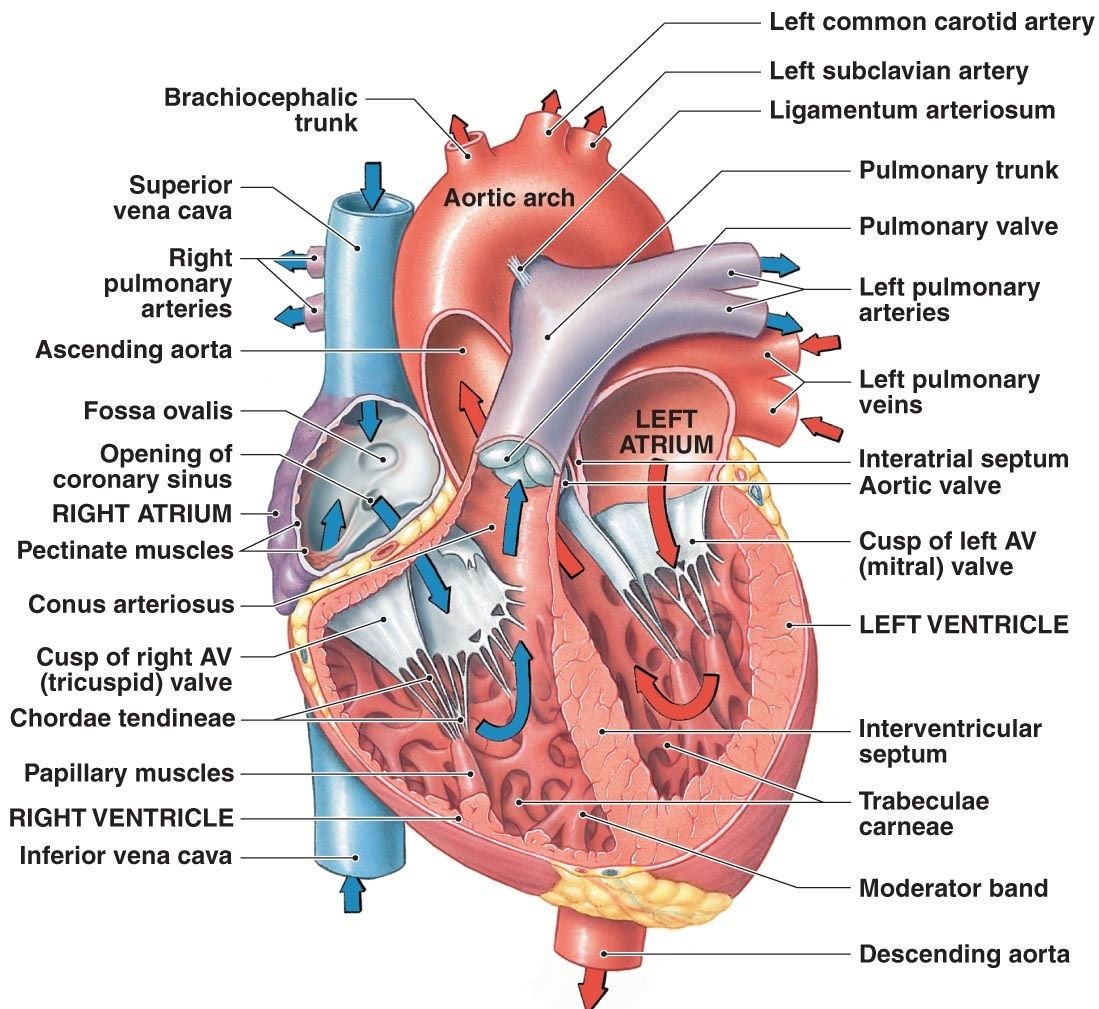
- Right-sided heart failure
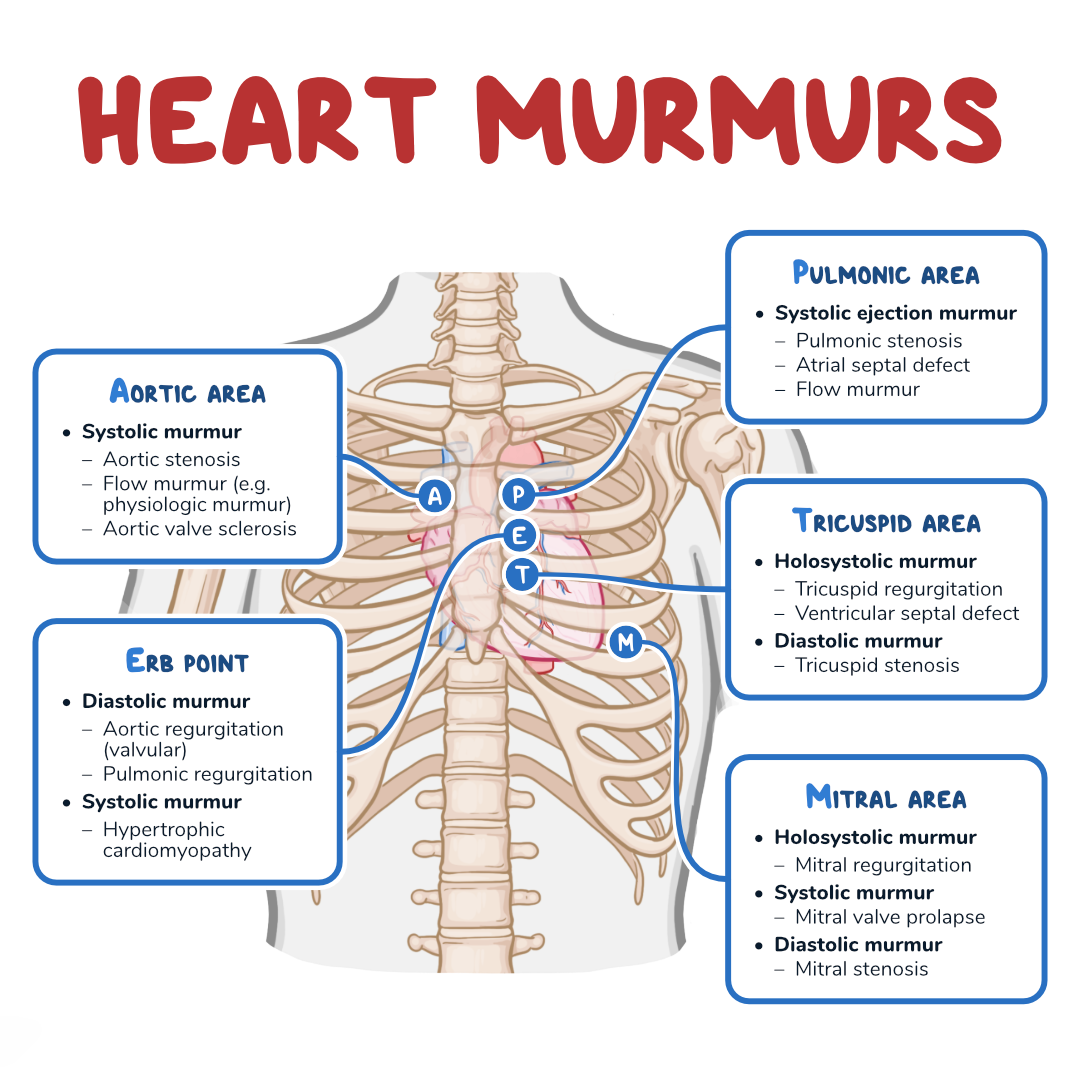
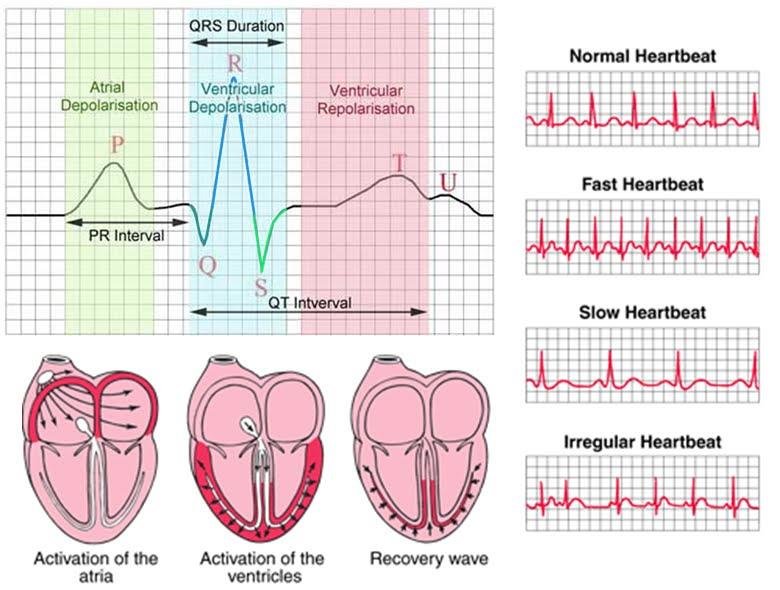
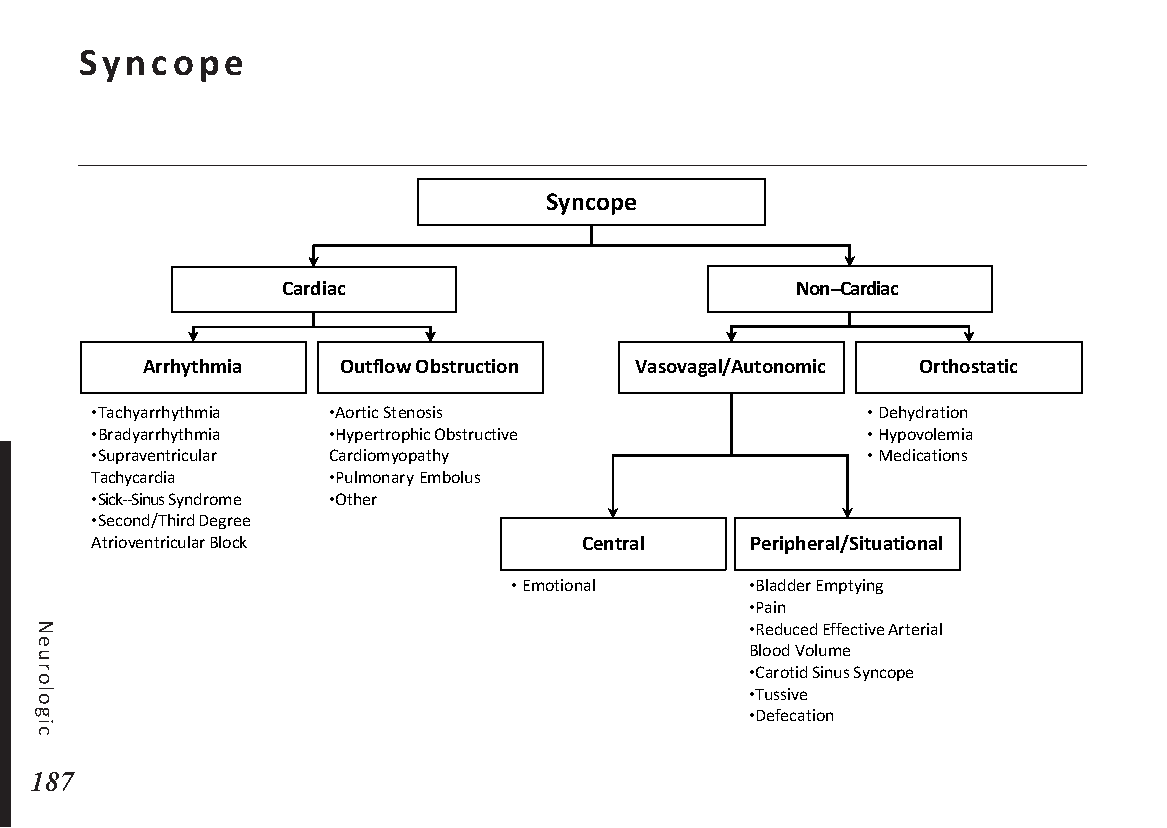
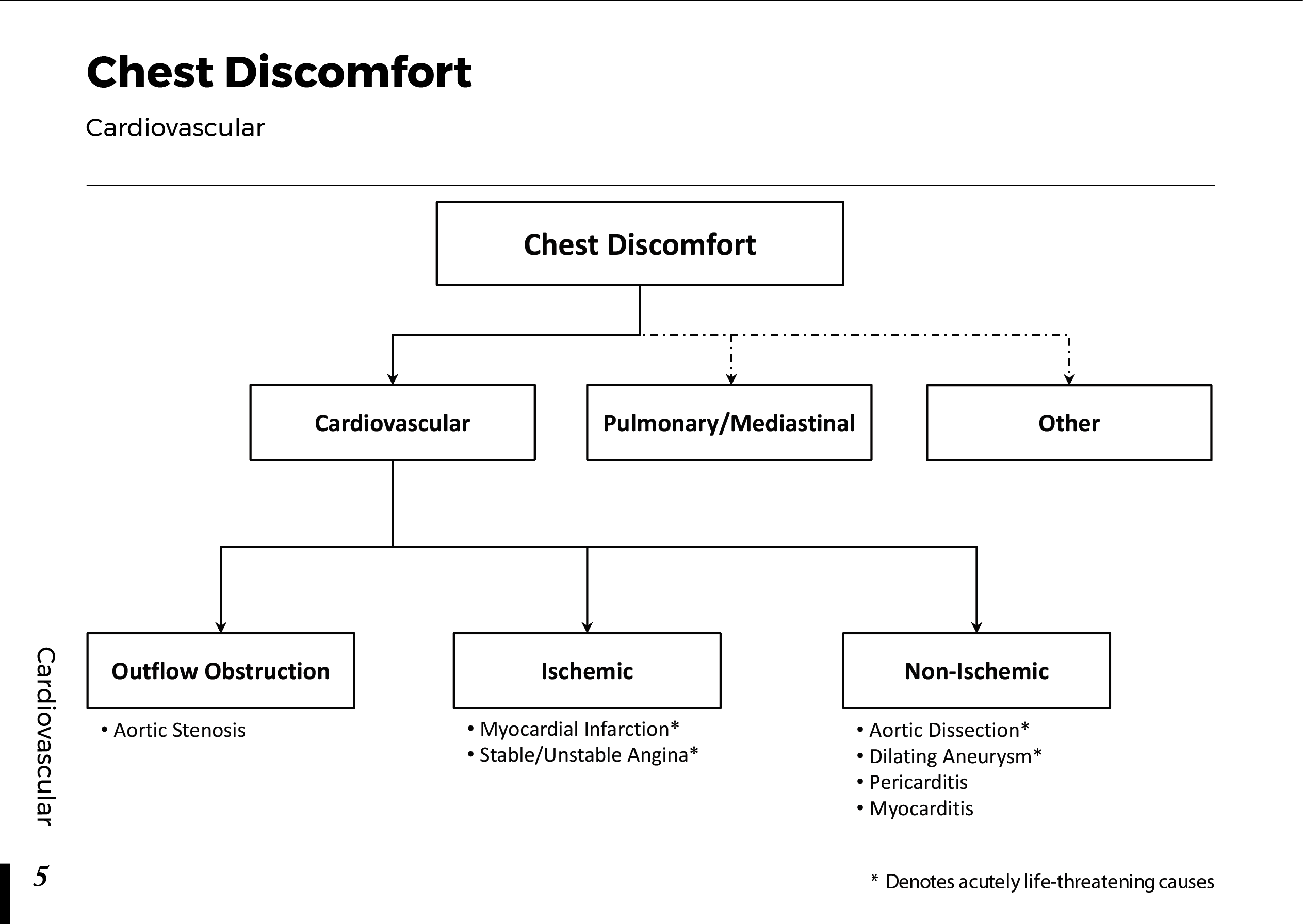
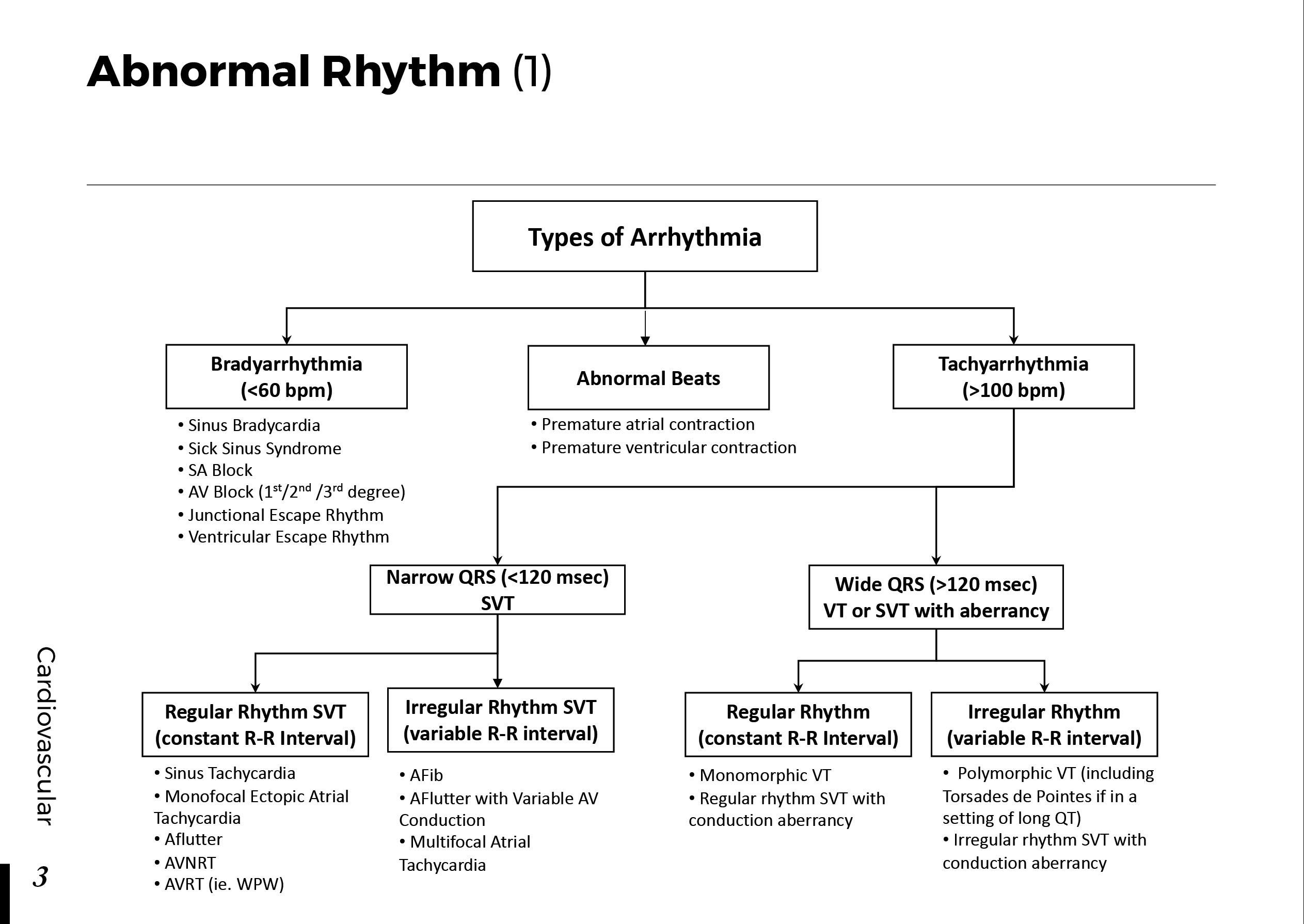
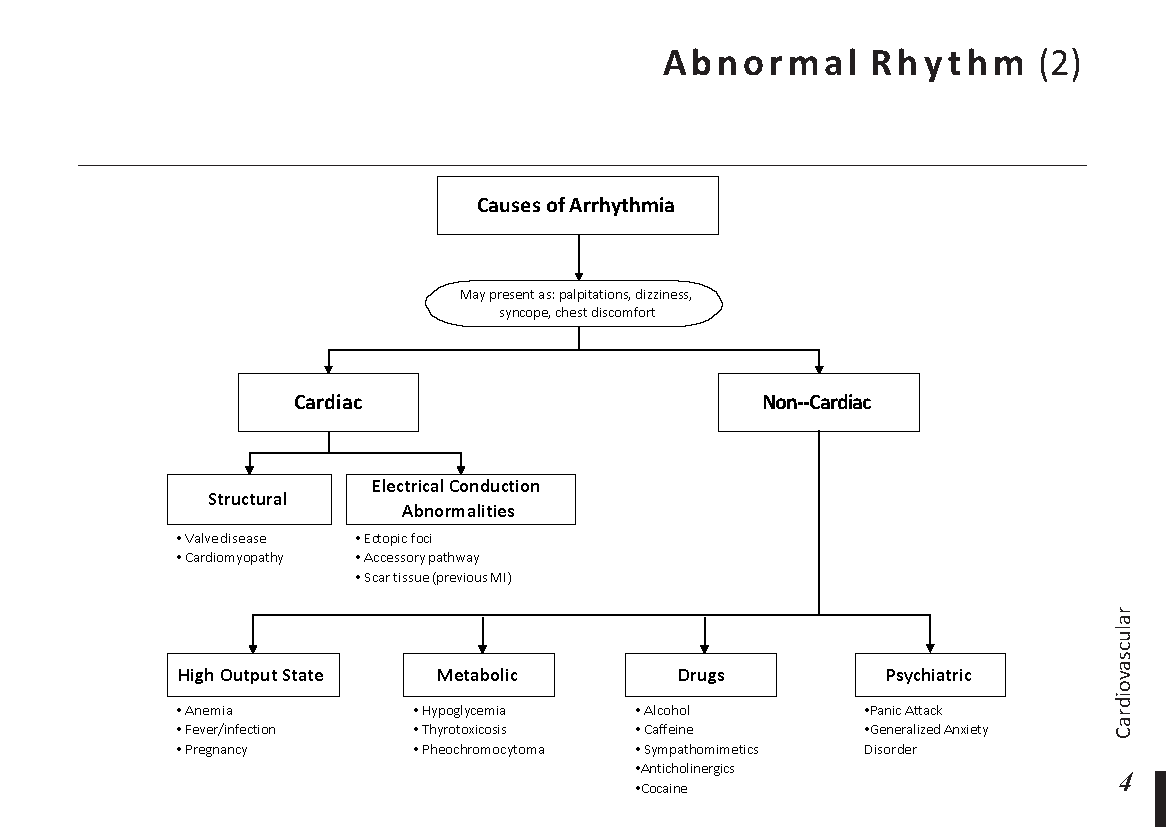
- Arrhythmias such as atrial fibrillation
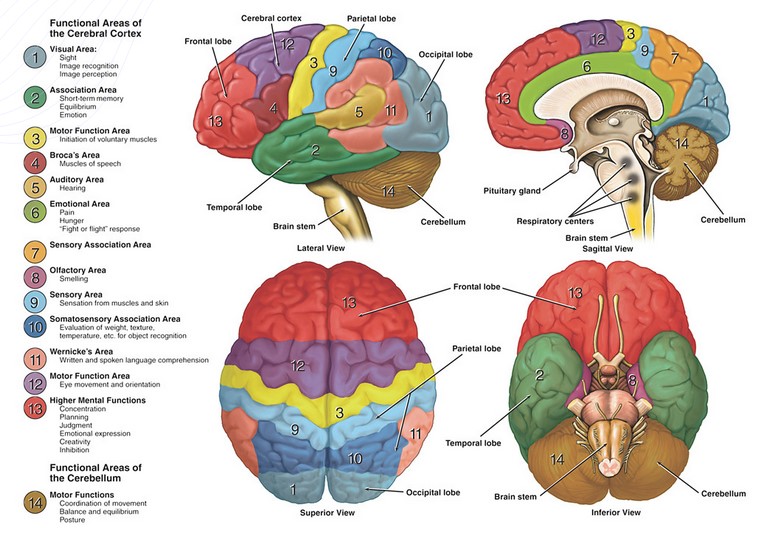
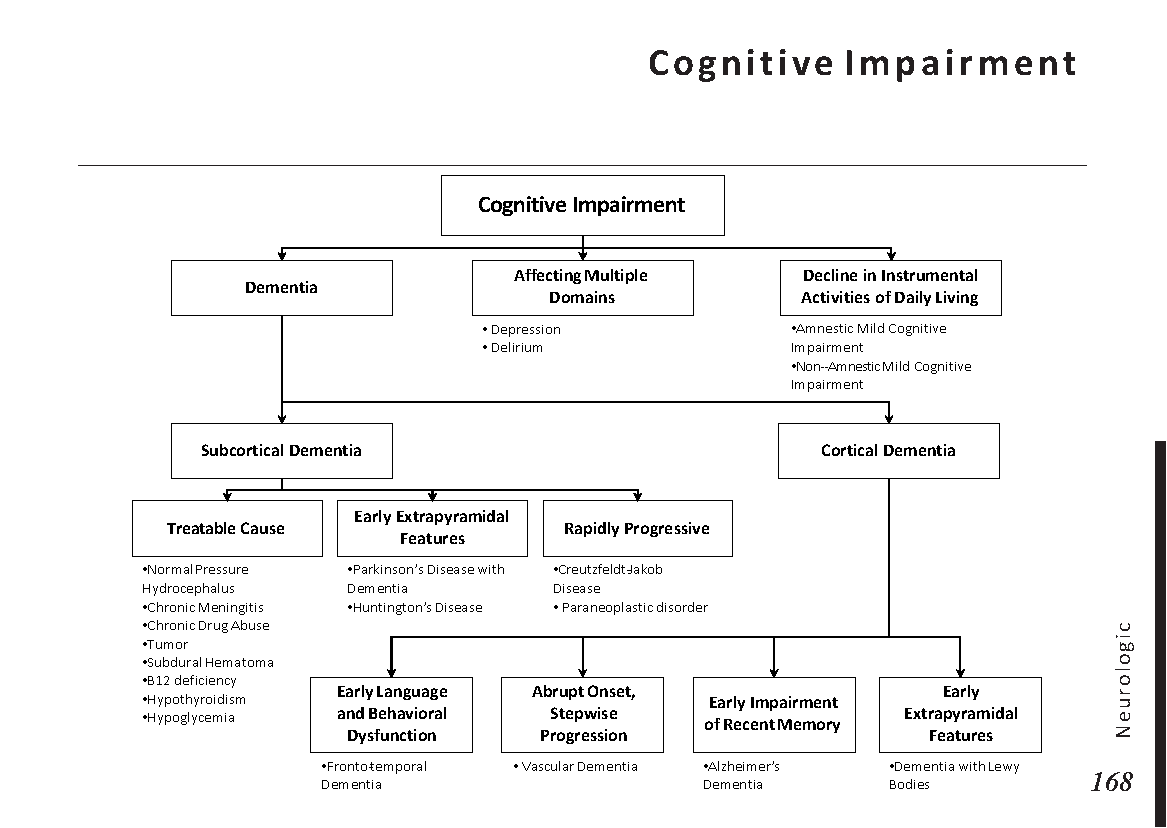
- Cognitive impairment due to its effect on mammillary bodies
- Increased risk of type 2 diabetes mellitus
When handled incorrectly, this can potentially spiral into a vicious circle. Fluid accumulates in the body as a result of right-sided heart failure, which can enhance the risk and severity of OSA by adding to the pressure in the area around the throat. This could then worsen the condition of chronic inflammation and cause heart failure.
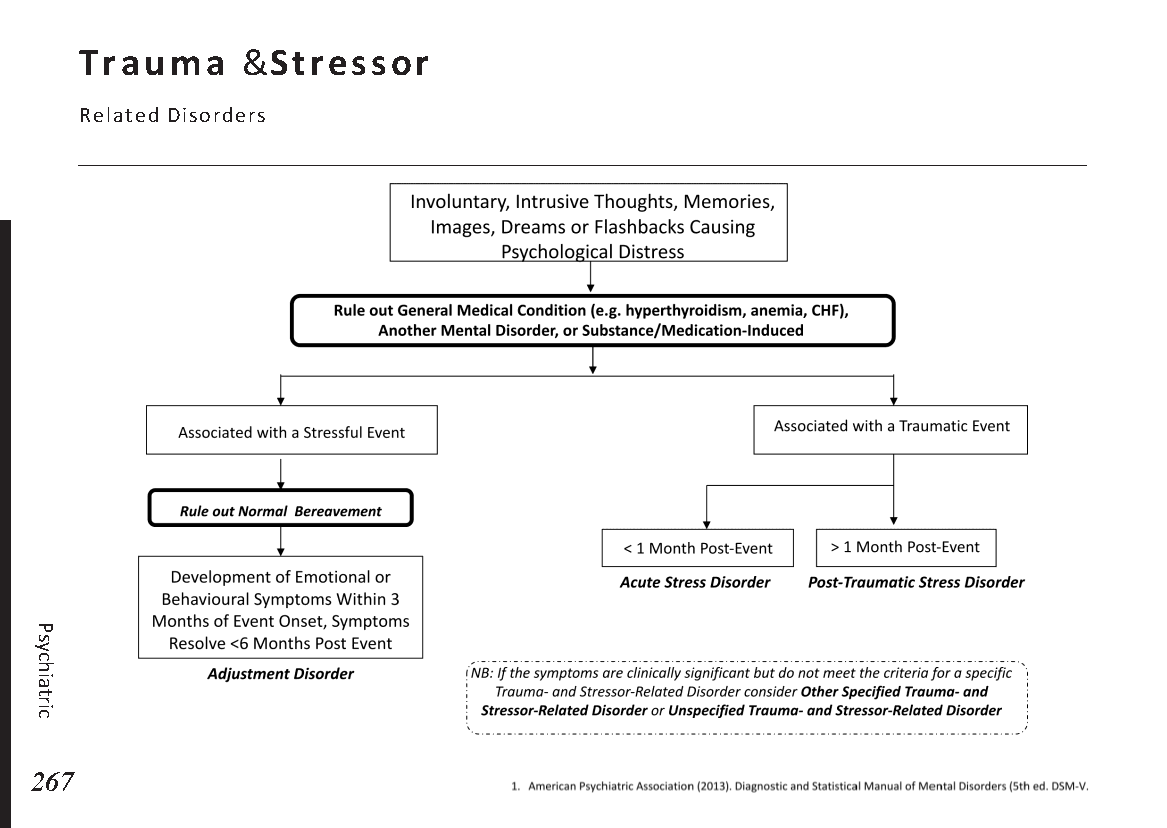
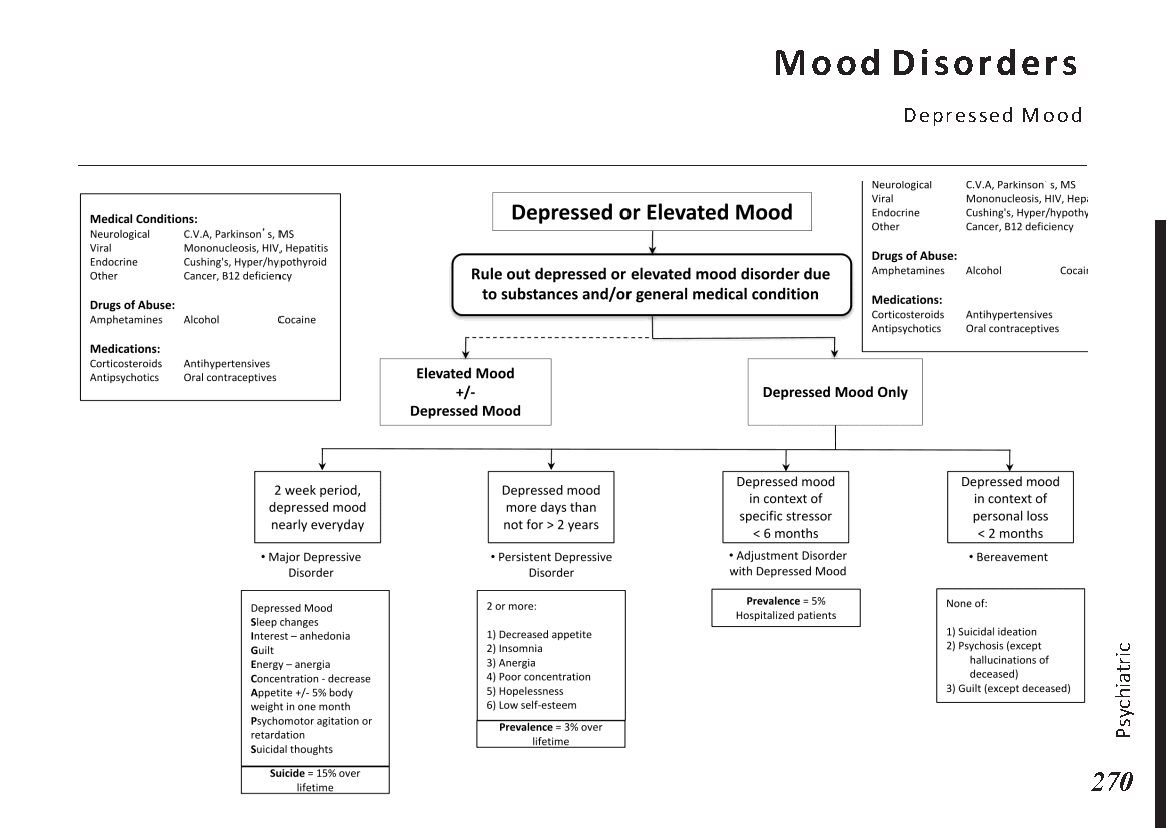
Poor-quality sleep has long-term effects as well. People who have trouble sleeping are more prone to experience anxiety and despair, and getting too little sleep raises the risk of:
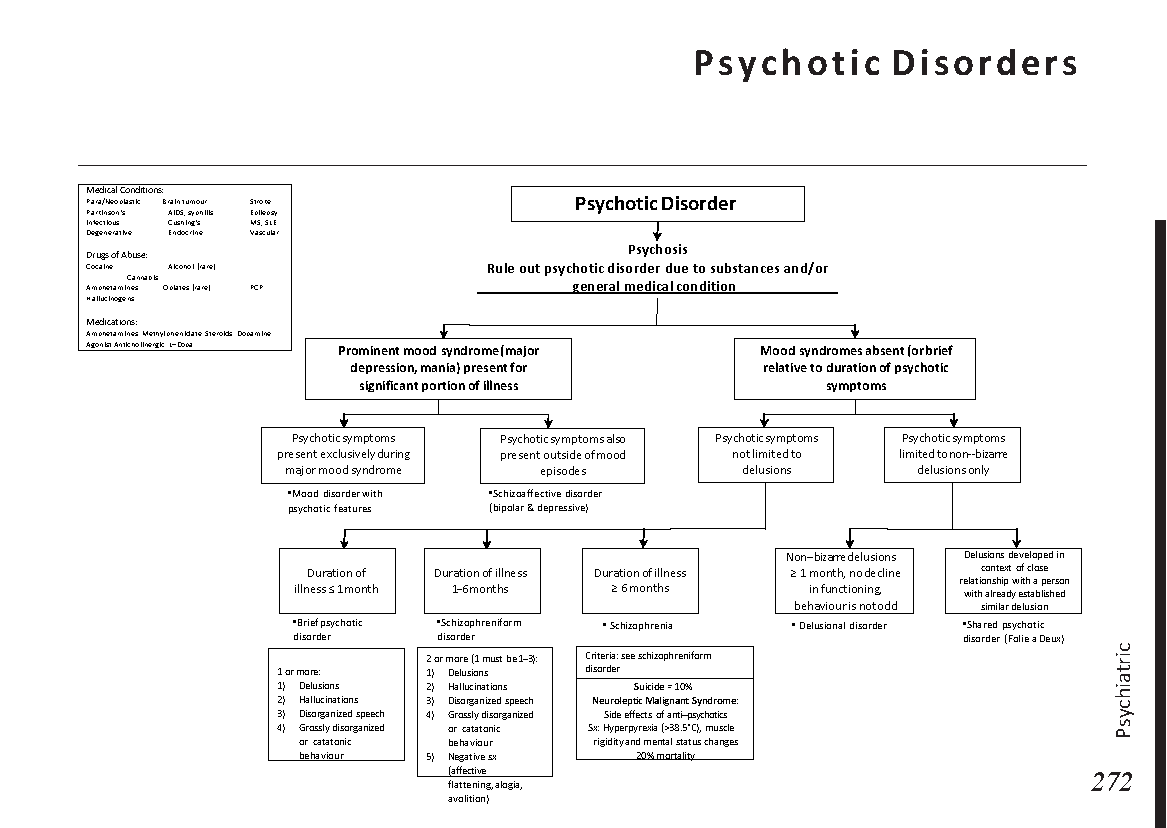
- Mania
- Psychosis
- Road traffic and workplace accidents
- An underproductive workforce
- Suicide
The burden on these patients’ mental health—who are already at risk for sadness and anxiety due to COPD—increases as their sleep quality deteriorates.
How to diagnose overlap syndrome?
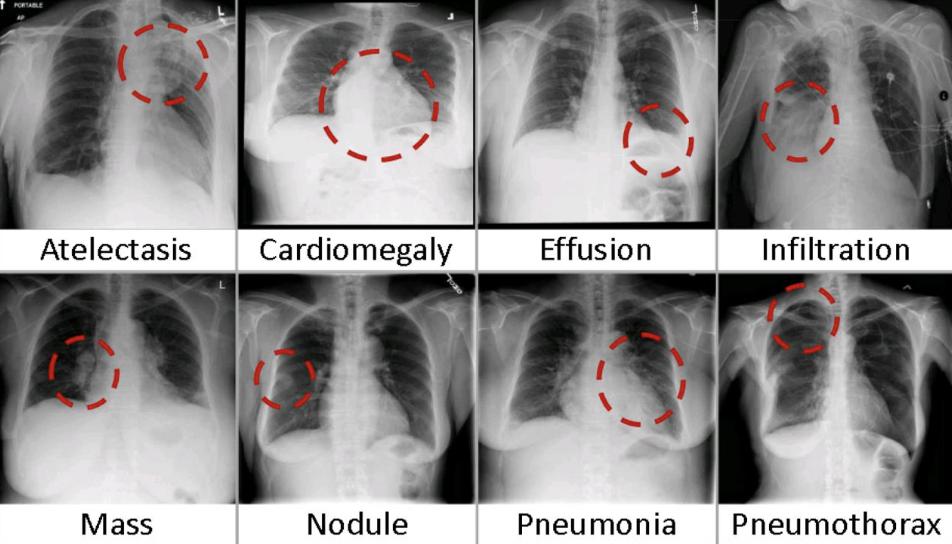
We must take into account a number of factors while approaching overlap syndrome, including the fact that both COPD and OSA are gravely underdiagnosed. According to studies, up to 70% of patients with COPD lack an official diagnosis, and up to 1 billion people worldwide—up to 50% of adults in some nations—suffer from OSA.
Screening people who already have a diagnosis of COPD or OSA may help identify those with overlap syndrome since both conditions require specialized equipment for diagnosis. We can add a pre-screening questionnaire into normal care to better allocate our resources because using specialized diagnostic equipment for this purpose would require large expenditures.
We must take into account a significant component while approaching Patients with OSA who might eventually undergo official COPD screening tests include:
– Patients who have smoked a lot or have been around a lot of toxic smells
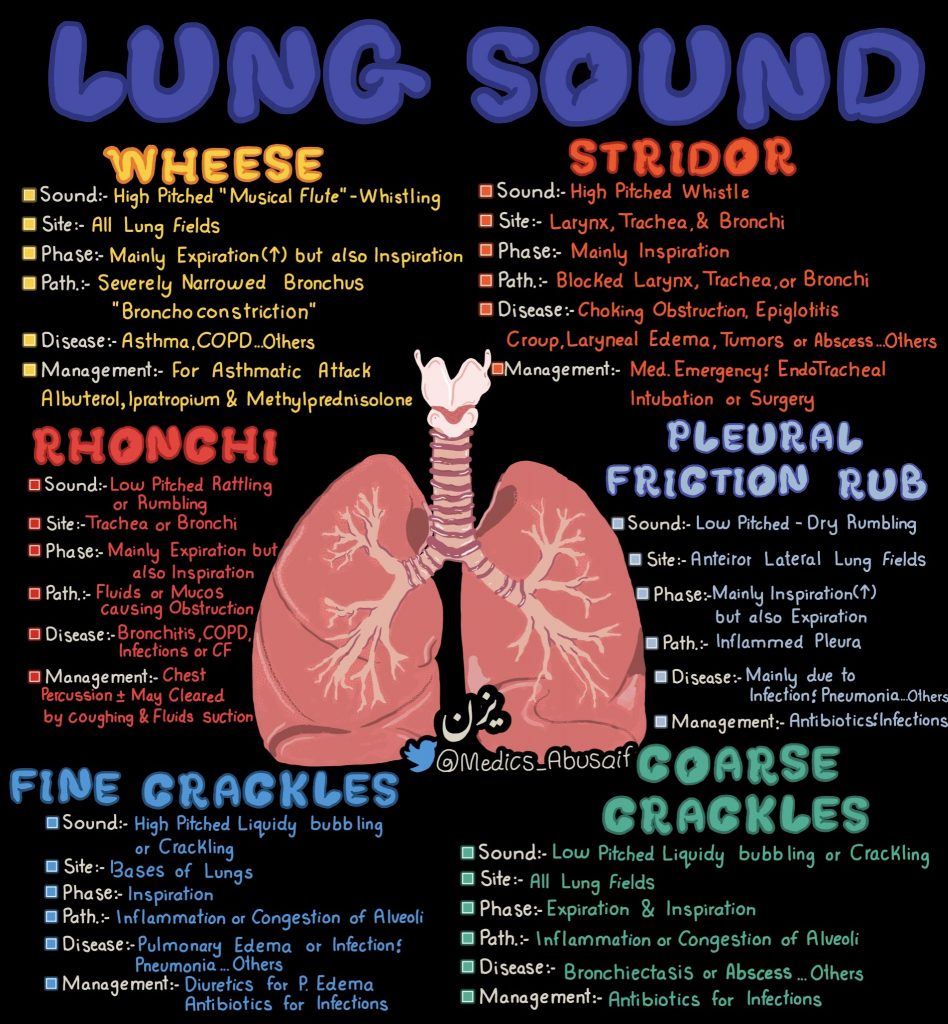
– Those whose examination reveals wheezing, pursed-lip breathing, or shortness of breath.
– Patients exhibiting symptoms that could be COPD symptoms include:
-Breathlessness
-Wheezing
-persistent phlegmy cough
-chest infections frequently
OSA screening is particularly challenging for COPD patients. It is significantly more difficult to distinguish between overlap syndrome and severe COPD when it comes to sleep complaints. This makes it possible to screen for OSA in all individuals with severe COPD. Patients with mild-moderate COPD who experience sleep symptoms that are out of character with the severity of their COPD may be eligible for formal screening tests, such as:
- Loud snoring
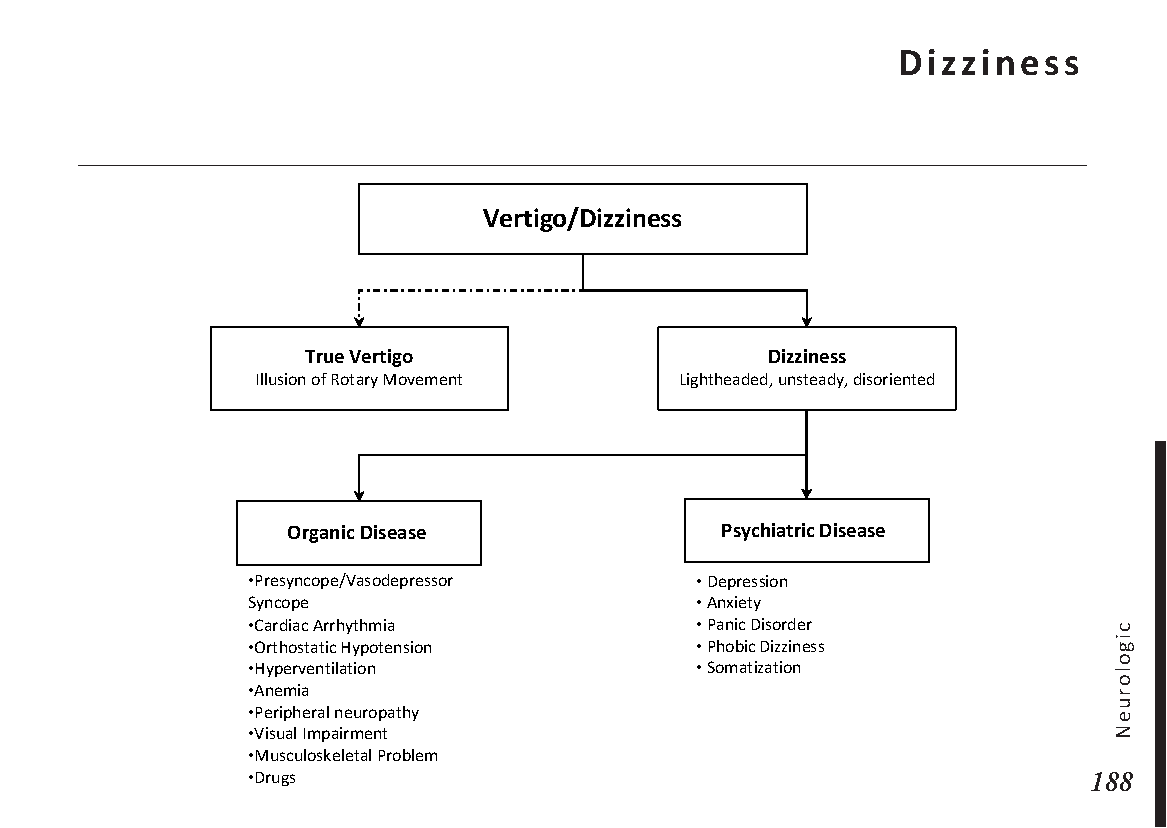
- Daytime sleepiness and difficulty concentrating
- Frequently waking during sleep
- Suddenly waking from sleep, gasping for air
- Dry mouth and sore throat after waking
How to treat overlap syndrome?
If overlap syndrome is identified, it is critical that the parent specialties of each disease—respiratory medicine and sleep medicine—cooperate to develop a strategy to lower the risks associated with this potentially fatal concoction. Because the medical field can sometimes advance slowly, we need to continuously educate the next generation of professionals about this uncommon illness.
Making sure COPD treatment is optimized and effective is the cornerstone of treating overlap syndrome. The patient uses CPAP (continuous positive airway pressure ventilation) every night to keep their oxygen levels stable while they sleep. CPAP works by continuously supplying high-pressure air through a face mask or nasal prongs. When the patient’s muscles relax during REM sleep, these devices help the airways stay open and the lungs cope better. Patients with overlap syndrome have a much lower mortality rate thanks to CPAP, which is frequently used as a treatment for OSA and severe COPD.
There has recently been discussion on whether NIV, which delivers air pressure through a mask that alternates between high and low pressure to help with breathing, provides any significant mortality benefits over CPAP. There is some resistance to changing recommendations because there is currently insufficient data to support making this the first-line treatment, despite some writers’ suggestions to the contrary.
Both disorders benefit from lifestyle changes, such as structured exercise programs and pulmonary rehabilitation, in addition to treatment with CPAP or NIV. To assist the patient’s lungs in making up for lost oxygen during sleep, these exercises improve fitness levels and strengthen chest wall muscles. Additionally, bronchodilators, corticosteroids, quitting smoking, and occasionally additional oxygen must be used to treat COPD as usual.
Finally, gastro-oesophageal reflux disease (GORD), which should be aggressively looked for and addressed by the treating provider, can be linked to and make OSA and COPD worse. Combining these terms yields the potential acronym COLDOSAGORD.

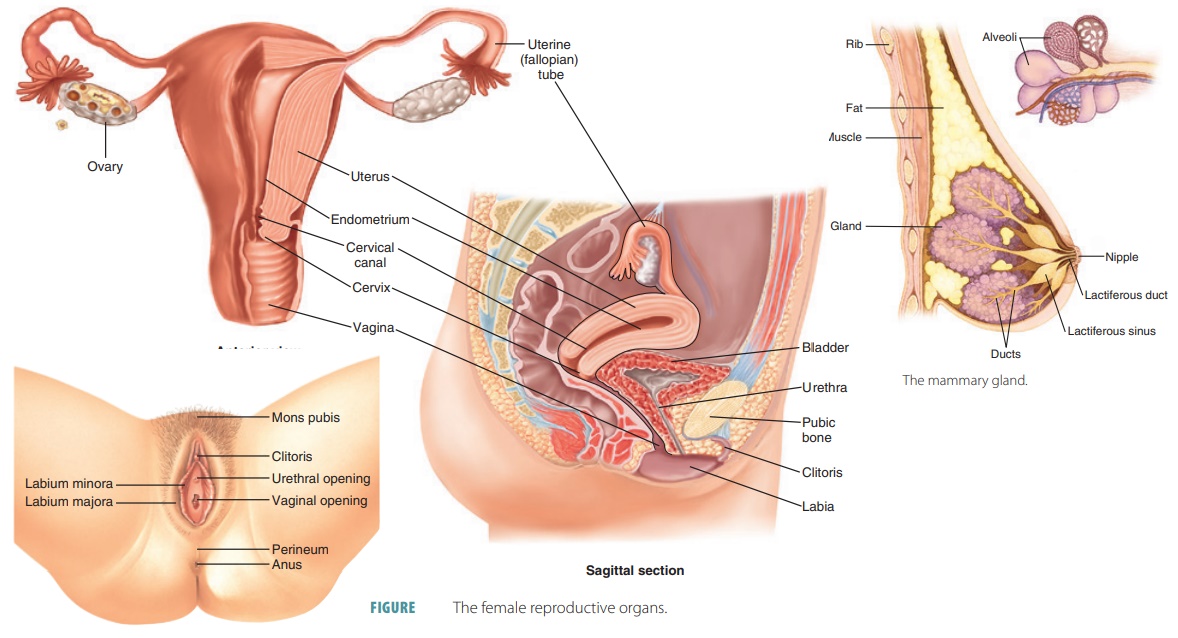 Menstrual cycle physiology:
Menstrual cycle physiology: